From News Medical
Promising new drug being developed for polycystic kidney disease
Researchers have developed a potential new drug for the treatment of Polycystic kidney disease (PKD) – a deadly genetic condition affecting the kidneys that leads to formation of swellings or cysts within the kidney that cause it to fail. The results of the initial animal testing of the drug have been published in the latest issue of the Nature Communications. The study is titled, “Discovery and preclinical evaluation of anti-miR-17 oligonucleotide RGLS4326 for the treatment of polycystic kidney disease.”
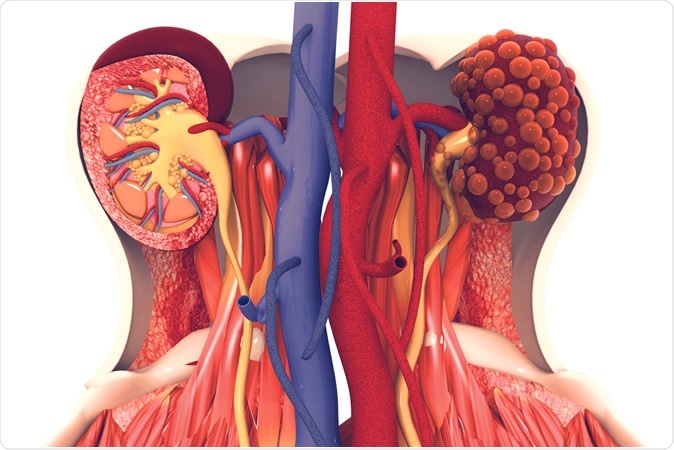
Kidney disease. 3d illustration, Credit: Crystal Light / Shutterstock
Dr. Vishal Patel, Associate Professor of Internal Medicine at UT Southwestern and senior author of the study explained that for this experiment they used lab mice and their potential new drug called the “anti-miR-17 oligonucleotide RGLS4326” was capable of reducing the kidney size by 50 percent among the mice models of PKD. Patel explained that PKD that is genetically inherited (also called Autosomal dominant PKD) affects around 12 million people globally and leads to end stage kidney failure by the age of 60 in many individuals. Patel said, “Once the kidneys have failed, the only options for survival are dialysis or a kidney transplant. A large percentage of ADPKD patients on dialysis die each year while waiting for a donated kidney.”
The authors wrote, “Autosomal dominant polycystic kidney disease (ADPKD), caused by mutations in either PKD1 or PKD2 genes, is one of the most common human monogenetic disorders and the leading genetic cause of end-stage renal disease.”
The researchers explained that ADPKD has a progressive course until the kidneys are swollen with the cysts and the organ fails. At present the only treatment available for PKD remains Jynarque (generically called Tolvaptan). Tolvaptan however is associated with a risk of severe liver damage says the label warning.
Dr. Patel said, “We earlier showed that levels of a tiny RNA fragment called microRNA-17 are increased in models of ADPKD. MicroRNA-17 interferes with the normal function of other, beneficial RNAs, causing kidney cysts to grow. RGLS4326, as the new drug is called in development, works by blocking the harmful microRNA-17.”
The authors explain, “Aberrant activation of miRNAs has been shown to promote the progression of multiple human diseases; therefore, miRNA inhibition has emerged as an attractive therapeutic strategy.” Stopping these miRNAs has been found to halt many diseases in their progression. They explain that “miR-17 miRNAs family is upregulated in both human and murine forms of ADPKD, and their deletion or inhibition attenuates cyst growth in mouse PKD models.”
The new molecule RGLS4326 is a short oligonucleotide inhibitor that stops microRNA-17 or miR-17. The molecule was developed from the screening of a large number (more than 190) of anti-miR-17 oligonucleotides from which it was found to be specific for inhibiting ADPKD. The early studies reveal that the molecule targets and accumulates in the kidney and the cysts present in the collecting ducts. At the level of translation within the cells, this molecule is capable of displacing the miR-17 and also stops the expression of Pkd1 and Pkd2 genes. This mechanism of action makes this new drug a potential therapy for ADPKD explain the researchers.
Thus the researchers came together to develop new therapies for this deadly kidney disease. The team from UT Southwestern and Regulus Therapeutics Inc. (the latter is a biopharmaceutical company in California that helped developed the molecule) collaborated on this study. The molecule was found to be delivered directly at the kidneys bypassing the liver and thus was found to be safe for the liver.
The study looked at in vitro preparations of kidney cysts and found the drug to be able to inhibit the growth of the cysts. It was then experimented on multiple mice PKD models after administering the drug subcutaneously by injection.
For the human cyst in vitro studies the team used cyst cultures from human ADPKD donors. RGLS4326 treatment was found to de-repress the mRNAs of predicted miR-17 target genes. Further the expression of miR-17 target encoded proteins polycystin-1 (PC1) and polycystin-2 (PC2) was raised by two times and four times respectively. The team next cultured the molecule with the cysts and found “significant reduction of in vitro cyst growth and proliferation in a concentration-dependent manner.” Overall the molecule was not toxic to the kidney cells that did not have ADPKD, the team noted.
Next the team used mice models to study the movement of the drug within a live system. Following a subcutaneous injection, the drug was found to be rapidly absorbed into the plasma and was found to reach the kidneys. The preference of the drug for the kidney in comparison to the liver was 13:8, the researchers wrote.
Now within mice models of ADPKD they noted the effects of RGLS4326. They found that the molecule when injected subcutaneously was capable of displacing miR-17 from polysomes within 24 hours. Peak displacement of the miR-17 was seen after a week and the effects persisted for up to two weeks, the team wrote. They injected the drug in both normal and PKD models of the mice at different doses and found that in both normal and PKD mice the displacement of the miR-17 was seen. In multiple mice models of ADPKD, the miR-17 inhibition was clearly proven with the new molecule. As a next step long term use of the drug was seen on mouse models and its safety and efficacy was established.
Regulus Therapeutics has started preliminary human phase 1 trials since last year. Meanwhile the drugs watchdog Food and Drugs Administration (FDA) has called for more information on the new molecules from the animal studies before human trials could be allowed to start said Dr. Patel. Authors concluded, “The preclinical characteristics of RGLS4326 support its clinical development as a disease-modifying treatment for ADPKD.”
The study was funded by Regulus Therapeutics and Dr. Patel also received funds by way of grants from the National Institutes of Health and the Department of Defense.
Kidney Transplants
Patients in the United States who receive dialysis at for-profit rather than nonprofit facilities are less likely to have access to kidney transplantation, according to a new report published in JAMA.
In a retrospective cohort study of 1,478,564 patients treated at 6511 dialysis facilities, Rachel E. Patzer, PhD, MPH, of Emory University School of Medicine in Atlanta, and colleagues found that receiving dialysis at a for-profit facility compared with a nonprofit facility was associated with a significant 64%, 48%, and 56% decreased likelihood of being placed on a deceased donor kidney transplantation waiting list, receiving a living donor kidney transplant, and receiving a deceased donor kidney transplant, respectively.
To the investigators’ knowledge, no previous studies have examined the relationship between dialysis facility profit status and both living donor or deceased donor kidney transplantation.
Dr Patzer’s team categorized dialysis facility ownership as nonprofit small chains, nonprofit independent facilities; for-profit large chains (more than 1000 facilities), for-profit small chains (less than 1000 facilities), and for-profit independent facilities. They referred to DaVita and Fresenius Medical Care as large for-profit chain 1 and large for-profit chain 2, respectively.
Of the 1,478,564 patients, 109,030 (7.4%) received care at 435 nonprofit small chain facilities; 483,988 (32.7%) received care at 2239 large for-profit chain 1 facilities; 482,689 (32.6%) received care at 2082 large for-profit chain 2 facilities; 225,890 (15.3%) received care at 997 for-profit small chain facilities; and 98,680 (6.7%) received care at 434 for-profit independent facilities.
Compared with patients who received dialysis at nonprofit small chain dialysis facilities, those treated at nonprofit independent facilities were almost 2.4 times more likely to be placed on the deceased donor transplantation waiting list, Dr Patzer and her collaborators reported. Patients who received dialysis at large for-profit chain 1, large for-profit chain 2, for-profit small chain, and for-profit independent chain facilities were 43%, 46%, 44%, and 40% less likely to be placed on the deceased donor transplantation waiting list, respectively
In addition, compared with patients receiving dialysis in nonprofit small chain dialysis facilities, those receiving dialysis at nonprofit independent facilities were 71% more likely to receive a deceased donor transplant, whereas patients treated at large for-profit chain 1, large for-profit chain 2, for-profit small chain, and for-profit independent chain facilities were 40%, 41%, 40% and 41% less likely to receive a deceased donor transplant, respectively.
Patients who switched from a nonprofit to a for-profit facility were more likely to be placed on the deceased donor transplant waiting list or receive a deceased or living donor kidney compared with patients who initiated and continued dialysis at for-profit facilities, Dr Patzer and her colleagues reported.
Patients who received dialysis at all for-profit facilities were 48% less likely to receive a living donor transplant compared with patients who were treated at all nonprofit facilities, according to the investigators.
In an accompanying editorial, L. Ebony Boulware, MD, MPH, of Duke University School of Medicine in Durham, North Carolina, and coauthors said findings of the new study, taken together, “paint a bleak and discouraging picture on the function of the dialysis industry in assisting patients’ access to kidney transplantation overall, and they draw a particularly concerning light on how the business practices of different dialysis organizations might influence patients’ access to life-enhancing therapy.”
Reference
Gander JC, Zhang X, Ross K, et al. Association between dialysis facility ownership and access to kidney transplantation. JAMA. 2019;322:957-973. doi: 10.1001/jama.2019.12803
Boulware LE, Wang V, Powe NR. Improving access to kidney transplantation: Business as usual or new ways of doing business? JAMA. 2019;322:931-933.
No comments:
Post a Comment