From Science Codex
Mini-kidney organoids re-create disease in lab dishes
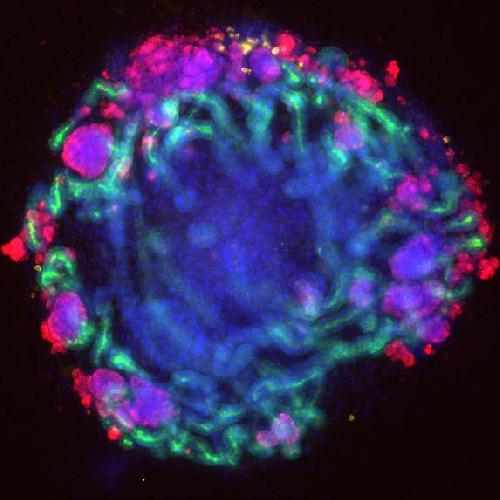
Mini-kidney organoids have now been grown in a laboratory by using genome editing to re-create human kidney disease in petri dishes.
The achievement, believed to be the first of its kind, resulted from combining stem cell biology with leading-edge gene-editing techniques.
The journal Nature Communications reports the findings today, Oct. 23. The work paves the way for personalized drug discovery for kidney disease.
The mini-kidney organoids were grown from pluripotent stem cells. These are human cells that have turned back the clock to a time when they could develop into any type of organ in the body. When treated with a chemical cocktail, these stem cells matured into structures that resemble miniature kidneys.
These organoids contain tubules, filtering cells and blood vessel cells. They transport chemicals and respond to toxic injury in ways that are similar to kidney tubules in people.
"A major unanswered question was whether we could re-create human kidney disease in a lab petri dish using this technology," said Benjamin Freedman, who led the studies at Brigham and Women's Hospital in Boston. He is now an assistant professor of medicine in the Division of Nephrology at the University of Washington and a UW Medicine researcher.
"Answering this question," he said, "was important for understanding the potential of mini-kidneys for clinical kidney regeneration and drug discovery."
To re-create human disease, Freedman and his colleagues used the gene-editing technique called CRISPR. They engineered mini-kidneys with genetic changes linked to two common kidney diseases, polycystic kidney disease and glomerulonephritis.
The organoids developed characteristics of these diseases. Those with mutations in polycystic kidney disease genes formed balloon like, fluid filled sacks, called cysts, from kidney tubules. The organoids with mutations in podocalyxin, a gene linked to glomerulonephritis, lost connections between filtering cells.
"Mutation of a single gene results in changes kidney structures associated with human disease, thereby allowing better understand of the disease and serving as models to develop therapeutic agents to treat these diseases," explained Joseph Bonventre, senior author of the study. He is chief of the Renal Division at Brigham and Women's Hospital and a principal faculty member at Harvard Stem Cell Institute.
"These genetically engineered mini-kidneys," Freedman added, "have taught us that human disease boils down to simple components that can be re-created in a petri dish. This provides us with faster, better ways to perform 'clinical trials in a dish' to test drugs and therapies that might work in humans."
The researchers found that genetically matched kidney organoids without disease-linked mutations showed no signs of either disease.
"CRISPR can be used to correct gene mutations," explained Freedman. "Our findings suggest that gene correction using CRISPR may be a promising therapeutic strategy."
In the United States, costs for kidney disease are about 40 billion dollars per year. Kidney disease affects approximately 700 million people worldwide. Twelve million patients have polycystic kidney disease and two million gave complete kidney failure. Dialysis and kidney transplantation, the only options for patients in kidney failure, can cause harmful side effects and poor quality-of-life.
"As a result of this new technology," Freedman said, "we can now grow, on demand, new kidney tissue that is 100 percent immunocompatible with an individual's own body."
He added, "We have shown that these tissues can mimic both healthy and diseased kidneys, and that the organoids can survive in mice after being transplanted. The next question is whether the organoids can perform the functions of kidneys after transplantation."
source: University of Washington Health Sciences/UW Medicine
Gift of Life
From Grand Island Independent, Nebraska, By Lauren Sedam

BURWELL — Korlyn Goff is the queen of casseroles.
Just ask her sister, Lisa Obermier.
It’s something Goff and Obermier said they learned from their mother, Dee Conner, when they were growing up in Burwell. Whether it was helping harvest crops or showing up with food in someone’s time of need, the sisters saw how important it was to be there.
“I live by the philosophy that you have to be a neighbor to have a neighbor,” Goff said.
But last year, Goff took that giving spirit above and beyond. Obermier had long been living with polycystic kidney disease, and she was in need of a donor. Goff stepped up, and almost a year later, the two are thriving. But to Goff, the gift wasn’t some heroic effort.
It was what she had to do for her sister.
“It was the right thing to do,” Goff said. “It was the only thing to do.”
Finding the match
Polycystic kidney disease is a disorder in which cysts form in the kidneys, causing complications, including kidney failure. It is hereditary, and several members of Goff’s and Obermier’s family have the disease, which can also present itself in the liver. Some have had transplants as well, and other family members have donated to some of them.
About 25 years ago, Conner was diagnosed with the disease in her liver. At the time, Obermier was tested, but her liver was fine. It wasn’t until about 10 years ago that Obermier, who now lives in York, discovered she had the disease in her kidneys.
“That’s when they said it leads to transplant or dialysis or death,” she said.
For a long time, Obermier was on the list for an “angel donor,” but a living donor was also an option.
It became more of a possibility for Goff, who still lives in Burwell and does not have the disease, when her sister was forced to go on dialysis. She saw her struggling, and she knew then that she had to get tested.
“I thought the sooner I make this decision, the sooner we can get on with life,” she said.
Other family members, including their father, Delmer, had wanted to donate, but Goff said she knew she was the match. Around Thanksgiving, she started the process. After ensuring she was current on a variety of exams and after having preliminary blood work done, Goff underwent more extensive testing at Mayo Clinic in Minnesota.
“They tested you from one end to the other in that two days,” she said.
At the end of it, Goff heard the news she’d always expected: She was a match. Those at Mayo Clinic told her to go home and talk about it with her family, but Goff knew what she needed to do.
Even so, others weren’t so sure.
Goff’s husband, Dave, is an only child, she said, and it was hard for him to think about his wife and the mother of Dustin, 26, and Kaden and Kortney, 21, going through something so big. For the Conners, it was hard to imagine both of their daughters in this situation. It was a scary time, Dee Conner said, but she knew Goff had her mind made up.
“She had told me that she thought it was something she needed to do to save her sister’s life,” Conner said.
Obermier, too, worried about putting her sister in danger.
"It was mixed feelings because it’s very humbling to have to accept that kind of gift from anyone,” she said. “And I’d rather be on the other end of it any day.”
Their biggest fears
The operation was set for Dec. 30. Goff, who works at a salon, wanted to recover during her slower months, and the transplant teams were able to make it work.
Obermier went to Minnesota on Christmas Eve for testing, and Goff came the day after Christmas.
On the day, they were supposed to be the second operation, but they were bumped to third. Goff was finally taken in at about noon, and Obermier was left to wait until they were ready for her a few hours later.
The sisters both came through the procedure, but they soon had a brush with some of their biggest fears. [Read more]
"It`s been a big gift," said Heather Watson-Vance, who received great news last week when she found out that her step-daughter Cori Vance was a match to be an organ donor. "I was born with polycystic kidney disease, which is a terminal genetic illness. There is no cure. Pretty much all we can do is a kidney transplant or dialysis," said Heather Watson-Vance.
So when she found out Cori was approved to be a living donor and give her a kidney, she was ecstatic; until she found out Cori's employer - Windsor Windows & Doors in West Des Moines - wasn't so thrilled.
Cori says she kept Windsor in the loop throughout the whole process, and told them that she was being tested to see if she was a match, but that when the company found out she was a match, she was met with opposition.
"The HR lady had said that they`ve been talking and we need to talk about the days off and if I would be coming back, and so she recommended that she would give me a week to come back," said Cori.
Cori says she was later told by Windsor that they would give her two weeks off tops, and that that was them being generous, and that there would be no restrictions. "I had informed them that, you know, I wasn`t gonna be able to come back without any restrictions, and what I do is the paperwork, that I would have a ten pound restriction, and then she asked me would you be able to stand? For 8-10 hours? and I said it`s all up to my doctor, like I don`t know right now and she said no, so she just told me that my last day would be October 30," said Cori. At her job, in addition to paperwork, Cori also moves metal. "I unload it and load it into a cradle," said Cori.
Channel 13 News went by Windsor Windows & Doors in West Des Moines to hear what they had to say about all of this, but we were told by the front desk that the Divisional Human Resources Manager - Pete Crivaro - had no comment. "And then I spoke with you guys and when you guys had showed up there, I don`t think he liked that very much. So, he told me that if I do speak with you guys to let him know so that he could prepare and that to let you guys know that he`ll grant me 4-6 weeks," said Cori.
But Cori and Heather say this story is bigger than just their situation. "And that`s not my point is for me to get the 4-6 weeks, because they weren't gonna give it to me anyways, until all of this happened. I just like, it`s not okay, and I don`t` want other people who like have thought about donating, I don`t want them to change their mind, not to do it because they're scared or companies aren`t giving them a chance neither," said Cori.
"We just really feel like with an organ donation that`s gonna impede other people from maybe wanting to donate an organ if they were treated this way at their job or they're not going to receive their job back after the donation, I mean you can`t put your own family in jeopardy, you know even to save a life," said Heather Watson-Vance. [Read more]
Fundraiser for Plainfield Boy in Need of Kidney Transplant

When five-year-old Drew Duszynski was born, he was diagnosed with a rare kidney disease and liver disorder: Autosomal Recessive Polycystic Kidney Disease and Congenital Hepatic Fibrosis.
On June 8, 2015 Drew had both of his oversized, diseased kidneys removed and after a month in the hospital he returned home. He receives nightly dialysis (10 hours) and, if all continues to go well, he will soon complete the transplant process and receive a new kidney.
Despite his condition and all the challenges, Drew is just a normal little boy – bright eyed, smart, sweet, playful, funny, inquisitive and full of life
With the total cost of a transplant often exceeding $500,000, transplant patient’s families are unable to shoulder the financial burden of such a procedure. While insurance will cover a great deal of the costs for Drew’s kidney transplant, the expected out-of-pocket costs are estimated to be in excess of $50,000.
In connection with the Children’s Organ Transplant Association, a fundraiser for Drew will be held from noon to 3 p.m. Saturday, Nov. 7 at Katie O’Connor’s Pint House and Eatery at 13717 US Route 30 in Plainfield.
The event will include raffle drawings and 50/50, kids activities, food and a cash bar. Tickets are available at the door. Families will pay $12 or $6 per person. RSVP by Nov. 3 and receive a discounted ticket price of $8 for families or $4 per person. To RSVP, contact Dave Duszynski at 773.251.8464 ordaveduz@ameritech.net or Sara Swenson at773.677.7360 or sararenae_1@yahoo.com.
COTA (Children’s Organ Transplant Association) is a national charity dedicated to organizing and guiding communities in raising funds for transplant-needy patients. The organization helps children and young adults who need a life-saving transplant by providing fundraising assistance and family support. COTA does not charge for its services and does not take a percentage of funds raised.
Find our more about Drew and COTA at COTAforAndrewD.com.
So when she found out Cori was approved to be a living donor and give her a kidney, she was ecstatic; until she found out Cori's employer - Windsor Windows & Doors in West Des Moines - wasn't so thrilled.
Cori says she kept Windsor in the loop throughout the whole process, and told them that she was being tested to see if she was a match, but that when the company found out she was a match, she was met with opposition.
"The HR lady had said that they`ve been talking and we need to talk about the days off and if I would be coming back, and so she recommended that she would give me a week to come back," said Cori.
Cori says she was later told by Windsor that they would give her two weeks off tops, and that that was them being generous, and that there would be no restrictions. "I had informed them that, you know, I wasn`t gonna be able to come back without any restrictions, and what I do is the paperwork, that I would have a ten pound restriction, and then she asked me would you be able to stand? For 8-10 hours? and I said it`s all up to my doctor, like I don`t know right now and she said no, so she just told me that my last day would be October 30," said Cori. At her job, in addition to paperwork, Cori also moves metal. "I unload it and load it into a cradle," said Cori.
Channel 13 News went by Windsor Windows & Doors in West Des Moines to hear what they had to say about all of this, but we were told by the front desk that the Divisional Human Resources Manager - Pete Crivaro - had no comment. "And then I spoke with you guys and when you guys had showed up there, I don`t think he liked that very much. So, he told me that if I do speak with you guys to let him know so that he could prepare and that to let you guys know that he`ll grant me 4-6 weeks," said Cori.
But Cori and Heather say this story is bigger than just their situation. "And that`s not my point is for me to get the 4-6 weeks, because they weren't gonna give it to me anyways, until all of this happened. I just like, it`s not okay, and I don`t` want other people who like have thought about donating, I don`t want them to change their mind, not to do it because they're scared or companies aren`t giving them a chance neither," said Cori.
"We just really feel like with an organ donation that`s gonna impede other people from maybe wanting to donate an organ if they were treated this way at their job or they're not going to receive their job back after the donation, I mean you can`t put your own family in jeopardy, you know even to save a life," said Heather Watson-Vance. [Read more]
Fundraising
From Plainfield Patch, Plainfield IL, by Scott Viau

When five-year-old Drew Duszynski was born, he was diagnosed with a rare kidney disease and liver disorder: Autosomal Recessive Polycystic Kidney Disease and Congenital Hepatic Fibrosis.
On June 8, 2015 Drew had both of his oversized, diseased kidneys removed and after a month in the hospital he returned home. He receives nightly dialysis (10 hours) and, if all continues to go well, he will soon complete the transplant process and receive a new kidney.
Despite his condition and all the challenges, Drew is just a normal little boy – bright eyed, smart, sweet, playful, funny, inquisitive and full of life
With the total cost of a transplant often exceeding $500,000, transplant patient’s families are unable to shoulder the financial burden of such a procedure. While insurance will cover a great deal of the costs for Drew’s kidney transplant, the expected out-of-pocket costs are estimated to be in excess of $50,000.
In connection with the Children’s Organ Transplant Association, a fundraiser for Drew will be held from noon to 3 p.m. Saturday, Nov. 7 at Katie O’Connor’s Pint House and Eatery at 13717 US Route 30 in Plainfield.
The event will include raffle drawings and 50/50, kids activities, food and a cash bar. Tickets are available at the door. Families will pay $12 or $6 per person. RSVP by Nov. 3 and receive a discounted ticket price of $8 for families or $4 per person. To RSVP, contact Dave Duszynski at 773.251.8464 ordaveduz@ameritech.net or Sara Swenson at773.677.7360 or sararenae_1@yahoo.com.
COTA (Children’s Organ Transplant Association) is a national charity dedicated to organizing and guiding communities in raising funds for transplant-needy patients. The organization helps children and young adults who need a life-saving transplant by providing fundraising assistance and family support. COTA does not charge for its services and does not take a percentage of funds raised.
Find our more about Drew and COTA at COTAforAndrewD.com.
Living with PKD
From Northampton Chronicle, United Kingdom

A talented young footballer is playing out her dream thanks to a generous sponsorship from a Northampton company.
Bethan Edgell, 11, from Buckingham, continues to fight a serious kidney disease, Autosomal Recessive Polycystic Kidney Disease (ARPKD), however she has been recognised by the MK Dons. And to help her realise her footballing ambitions, pump specialist firm Process Systems International (PSI) has agreed to pay for her elite training.
The football crazy youngster plays for Moretonville Harriers as a Striker and is now training with the MK Dons Girls Skills Elite Centre U13 squad.
Her proud dad Chris, who is an engineering co-ordinator for PSI, said: “Bethan has to overcome so many health hurdles to play her various sports, that this opportunity is really important and rewarding for her. There is no cure for her condition and her kidneys will gradually deteriorate, so she is determined to make the most of every sporting opportunity given to her.
“To have the support of PSI to pay for her additional training is very touching indeed.”
As for Chelsea loving Bethan, it’s early days but so far she is enjoying her elite status. She said: “I am truly grateful to PSI for giving me this opportunity with the MK Dons. The various sports I play, in particular football, is a large part of my life and keeping fit is helping with my condition.”