From ABC Action News, Tampa Bay, FL, by Ashley Yore
We have a heartwarming update to a story we first told you about back in 2015. You may remember, a Tinder date, not making a love connection, but brining together a kidney donor with a woman in desperate need. That kidney recipient is doing much better, but the fight to cure Polycystic Kidney Disease is still going strong.
Richard O’Dea just ran the Boston Marathon.
“When there’s pain, you’re struggling through the race, and you think about all the people that you run for,” O’Dea said.
One person he’s running for is Erika Bragan, a close friend with Polycystic Kidney Disease, who received a badly-needed kidney back in 2015. O’Dea helped make that donation happen.
“I can’t believe it, I mean I still sit here and I have the most beautiful kidney put into my body from someone I did not know,” Bragan said.
That donor was someone O’Dea met on Tinder, and while their romantic relationship didn’t last, Bragan got a new kidney and a close friend.
“Now it’s just, it’s a whole new world,” she said.
“I like to think I was in the right place at the right time,” O’Dea said.
“It’s amazing to me to have someone just put not only their time and effort but a piece of them out there and say this is how I’m going to help you have a better life,” Bragan said.
Now that life is much better, the fight to cure PKD continues. O’Dea will run another marathon in Chicago in October.
“I don’t know if its fate it’s hard to describe but it’s definitely a blessing in my life,” O’Dea said.
Team Tampa PKD will also be involved with the Walk for PKD at Fort Desoto Park October 14, 2017.
Since inception, they have competed in 9 major marathons as part of the Run for PKD and raised $140,000 for the PKD Foundation.
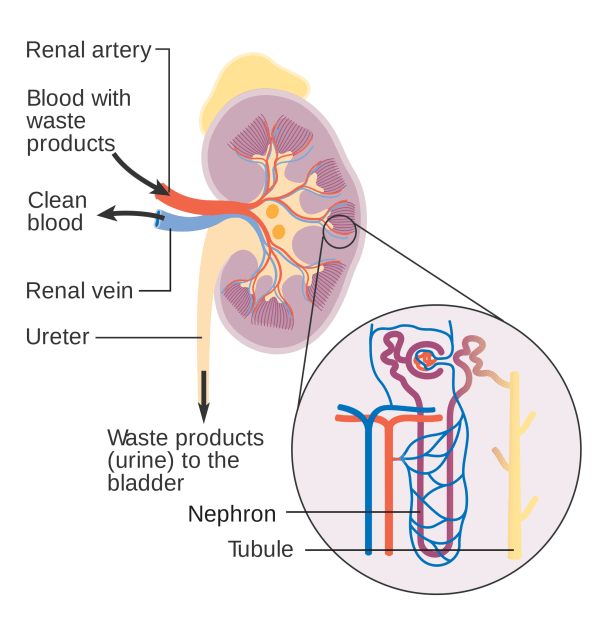
Living with PKD
From The Express Tribune
MADRID:
Juan Benito Druet has just learned that his life may be about to change. In the next few hours he will receive a healthy kidney thanks to a pioneering system that has made Spain the world leader in organ transplants for the past 25 years.
“We don’t know what will happen. but you have to take a chance,” said Druet, 63, a reserved and moustachioed boilermaker, as he lays in his bed at Madrid’s La Paz hospital. Hospital staff try to reassure him by telling him organ transplants are carried out every day in Spain.
FIA empowered to curb human organ trafficking
Doctors performed 4,818 transplants last year, including 2,994 kidney transplants, according to the health ministry’s National Transplant Organisation (ONT). That means there were 43.4 organ donors per million inhabitants last year, a world record, up from 40.2 donors in 2015. By comparison in the United States there were just 28.2 donors per million inhabitants in 2015, 28.1 in France and 10.9 in Germany, according to the Council of Europe.
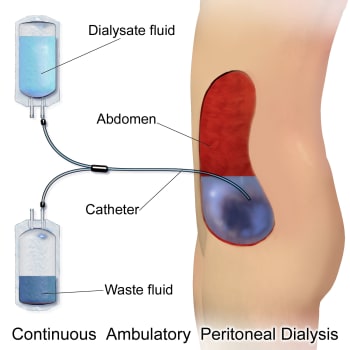
“It is even better than if we had won the jackpot in the lottery,” says Druet’s wife Jeronima, 60, as she sits close to him along with the couple’s two adult children. Now she dreams of going on a cruise with her husband, something impossible as long as he needed to be hooked to a 15-kilo kidney dialysis machine every night to filter his blood.
The transplant operation lasts four and half hours. Surgeons make a 15-centi metre incision in Druet’s abdomen to transplant a healthy kidney extracted the night before from a woman who died.
After a transplant patients “start to regain weight, their health improves. It is as if we transplant lives,” the founder of the ONT, Rafael Matesanz, tells AFP.
Matesanz oversaw the implementation of a centralised and well-oiled organ donation and transplant system which has been replicated in Portugal and Croatia and inspired others across Europe. Each hospital has a transplant coordinator, usually a doctor or nurse who specialises in intensive care, charged with identifying patients at risk of a heart attack or brain death. In both situations kidneys, livers, lungs, pancreas and sometimes even the heart can still work and can be transplanted.
Illegal Kidney Trade: Two suspected organ traffickers held
Organ donations are quickly reported to the ONT which searches for the best match from its organ waiting list. If the patient is far away, a cooler with the organ is sent by plane inside the cockpit with the pilot.
The operation is free under Spain’s public health system, anonymous and available only to residents of the country to avoid organ trafficking.
“What makes the difference is the organisation of the system. This network, this centralisation, is the key,” says Marie-Charlotte
Bouesseau of the World Health Organisation’s department of ethics.
Worldwide only about 10 per cent of all patients who need a transplant receive a donated organ, she adds. “That means that 90 percent will die while they are on a waiting list,” she explains. In Spain only four to six per cent of patients died in 2016 while they were on a waiting list for a vital organ – a liver, heart or lung.
Ramon Garcia Castillo, 85, a former TV technician, spent 13 months on dialysis before he received a kidney transplant in 2010. He would previously trek to a hospital three times a week to be hooked up to a machine for three-and-a-half hours. The kidney transplant “gave me my life back”, says Castillo, who now just needs to take pills to ensure his body does not reject the donated kidney.
The other secret to the success of the Spanish system is training and communication, explains Matesanz. Since it was set up in 1989, the ONT has trained over 18,000 transplant coordinators who break the news of a person’s death and then gently convince their loved ones to agree to donate their organs.
Scientists discover new organ in human body
Spanish law presumes consent for organs to be removed on their death unless they had previously made clear that they were against donation. But loved ones are systematically consulted.
“You have to have a lot of empathy, sensitivity, respect,” says Belen Estebanez, the transplant coordinator at Madrid’s La Paz hospital.
The work of a transport coordinator was depicted in Spanish director Pedro Almodovar’s 1999 Oscar-winning movie “All About My Mother”. The director consulted with the ONT to prepare the movie.
“If they have a lot of doubts we ask them what the person was like, if they were generous. From there we get them to reflect on an organ donation,” adds Damiana Gurria, another transplant coordinator. “It comforts many families to know that the organs of their loved ones will live on inside someone else, that people will be thankful for the rest of their lives.”
Castillo said he drinks two litres of water each day and follows a balanced diet since he received his new kidney. “I have to take care of it, especially since it was given to me. I have to be thankful.”
From DovePress, by Luca Degli Esposti, Chiara Veronesi, Valentina Perrone, Stefano Buda, Antonio Santoro Clicon S.r.l. Health, Economics & Outcomes Research, Ravenna, Italy; Department of Nephrology and Dialysis, Policlinico S. Orsola-Malpighi, Bologna, Italy
Objective: The aim of this study was to assess healthcare resource consumption and its associated costs among patients with polycystic kidney disease (PKD) in a real-world setting.
Methods: An observational retrospective cohort analysis was conducted using data from the administrative databases of four Italian local health units. Data for patients who were diagnosed with PKD during the inclusion period (January 1, 2010 to December 31, 2012) were extracted. The date on which a patient’s first PKD hospitalization occurred during the inclusion period was defined as the index date (ID), and the ID was defined as the date of the first dialysis treatment recorded during the inclusion period for patients undergoing dialysis. Data regarding the clinical characteristics of patients included in the study during the 12 months prior to the ID (pre-ID; characterization period) were collected. All patients were then followed up for the 12 months following the ID (post-ID; follow-up period). Healthcare consumption and its associated costs were analyzed during the follow-up period. All costs are reported in euros (€).
Results: A total of 1,123 patients with PKD were included in this study, 61.9% of whom were male; the mean age of the patients was 57.7±24.5 years. At diagnosis, 11.2% and 1.1% of patients were affected by the dominant and recessive forms of PKD, respectively. Approximately 8% of the included patients were undergoing dialysis at ID (baseline). The incidence of dialysis was fourfold greater among patients with autosomal-dominant PKD (ADPKD) than among the total cohort (33.3% compared with an overall 8.3%). During the follow-up period, the average annual rates of healthcare resource consumption were greater among dialyzed than non-dialyzed patients. The average healthcare expenditures were €45,059.62 and €3,913.89 (p<0.001) per year for dialyzed and non-dialyzed PDK patients, respectively. Our findings suggest that in the real-world Italian context, consumption of healthcare among patients with PKD has increased at dialysis initiation due to the cost of outpatient specialist healthcare services as well as other costs. Research on the prevention of PKD-related complications and disease progression may help to facilitate a decrease in the costs associated with this condition.
From The Boston Globe, By Felice J. Freyer
Catherine Burgoyne hated what was happening to her. At the age of 92, she had suddenly lost her cherished independence. A fall led to kidney failure, which led to dialysis, which led to the need to tie her wrists to the hospital bed rails.
In those days, she was often confused and would try to rip out the tube in her chest, implanted to enable dialysis. But her words and grimaces left no doubt that she could not bear the restraints, or her complete dependence — a life so different from what she had known just weeks earlier.
Burgoyne had chosen her nephew and his wife, Robert and Nancy Tucker, to make health care decisions if she could not. Now, her nephew spent hours at her side, distraught over her misery, anguished by the choice before him. Her hands could be freed if dialysis stopped. But dialysis was keeping her alive.
She was among the growing number of very old and very sick people who end up on dialysis, a procedure that filters toxins and other substances from the blood.
But as more elderly people suffer kidney failure, new data reveal a troubling pattern for dialysis patients: A high percentage die anyway, and even those who live longer often don’t live well. That has led some patients and doctors to consider what once might have been unthinkable: disconnecting the dialysis machine.
“We used to think, ‘Dialysis, it’s great. You get more life. You get more days. Let’s do it,’ ” said Jody Comart, director of palliative care for Hebrew SeniorLife, a Greater Boston nonprofit that provides an array of services to aging patients. “But now we understand, ‘Well, you get more days. But three days [a week] are taken up by dialysis and exhaustion and feeling crummy and you are likely to have several hospitalizations each year due to complications.’ ”
Dr. Ernest Mandel, medical director of nephrology and dialysis at Hebrew SeniorLife, said that too often dialysis is the default response to kidney failure, occurring without discussion. Patients have no idea what they’re getting into — or that they could choose another route.
Most cases of kidney failure in this country are caused by diabetes and hypertension, conditions that erode kidney function gradually over many years. Burgoyne’s illness was more sudden.
Alone in her apartment in a Foxborough senior housing project, she fell one night about a year ago. By the time a neighbor found her, she had been lying on the floor for a day or two. During those long hours without food or water, her muscles broke down and released toxins that damaged her kidneys.
She was admitted to a hospital intensive care unit, bruised and disoriented. As so often happens, Burgoyne started dialysis in a crisis — doctors call it “crashing into dialysis.” There was hope it would be temporary, that her kidneys might revive.
After a couple of weeks in the hospital, Burgoyne was admitted to the medical acute care unit at Hebrew SeniorLife, which takes care of people too sick for a nursing home but not needing a full-service hospital. Although she’d been living independently, she had a heart pacemaker, chronic obstructive lung disease, and high blood pressure, among other ailments, said Anne Carr, a nurse practitioner who cared for her at HebrewLife.
As the weeks went by, the hope for improvement waned. “We didn’t know if there was a recovery in her future,” Carr said.
Burgoyne’s wrists were tied to the bed rails all the time, because she was in danger of ripping out the permanent catheter needed for her three-times-a-week dialysis.
Tucker talked to his aunt about ending dialysis. “Do you understand what it means if we stop this? This is what is keeping you alive.” She responded with a kind of shrug, which he took to mean, “It is what it is, nothing I can do.”
In 2014, some 420,000 Americans were on dialysis at any given time, and that number has almost surely increased. Those older than 75 are the fastest-growing group of dialysis patients. Medicare spends about $88,000 annually per patient for dialysis and related services.
Dialysis has long been considered a necessary response to kidney failure, a life-saving and life-prolonging procedure. The patient’s blood is passed through a machine that removes electrolytes, toxins, and excess fluid. Younger people who are otherwise healthy can have full lives and even hold jobs while on dialysis.
Although the dialysis machine filters the blood, it doesn’t do as good a job as real kidneys. It often doesn’t even relieve the symptoms of kidney failure, which can include nausea, shortness of breath, muscle cramps, itching, tiredness, and lack of appetite. In many, dialysis induces a bone-deep fatigue. Patients also have to travel to a clinic three times a week, and spend three or four hours hooked to the machine.
To make matters worse, older people and people with multiple illnesses are prone to infections, clots, and other problems that can lead to repeat hospitalizations. Often, their health declines, and they lose the ability to manage daily activities such as bathing.
No wonder surveys have found that a majority of patients on dialysis regret starting it.
Dr. James A. Tulsky, chief of the division of palliative medicine at Brigham and Women’s Hospital, said he worries many dialysis patients would choose otherwise, if they were better informed at the outset.
“The typical answer is, ‘What else can I do?’ The answer is, there might be other options . . . and if you don’t like it, you may have the option to stop it,” he said.
A 2012 study of patients with end-stage kidney disease found that those who underwent dialysis lived 404 days longer than those who decided against the procedure. But 326 of those extra days were spent undergoing dialysis, and an uncounted number were lost to hospitalization.
Notably, for those older than 75, dialysis does not always result in any additional days of life. Studies in the Netherlands and the United Kingdom have shown that elderly patients who forgo dialysis often live about as long as those who choose the procedure.
American kidney doctors — known as nephrologists — need to change their approach, said Mandel, the Hebrew SeniorLife nephrologist. “We tended to wash our hands of the patient if they didn’t want dialysis,” he said.
Instead, he said, the decision should not be a matter of accepting or rejecting dialysis but choosing among transplantation, dialysis, or what is known as “conservative management” — a method of treating kidney disease focused on relieving symptoms and adjusting medications and lifestyle to preserve kidney function.
And then, he added, patients need to have continuing conversations about whether to change course. Stopping dialysis can be a weighty decision. Patients whose kidneys have become dependent on dialysis die quickly when it is withdrawn, within seven or eight days on average.
Although dialysis is expensive, the question of whether conservative management saves money has not been adequately studied. In any case, Mandel said, the main point is to improve patients’ quality of life.
Mandel thinks the decision to put Burgoyne on dialysis after her fall was reasonable, given the severity of her kidney failure and the hope for recovery. But, he said, she might have benefited from a conversation about what dialysis would entail and when to consider stopping it.
Once she was admitted to Hebrew SeniorLife, Burgoyne and her nephew had a chance for many conversations about her options. They were offered a service that few kidney patients get — palliative care, a team-based approach to managing serious illness that focuses on quality of life.
Palliative care is similar to hospice in that it works to treat symptoms and keep patients comfortable, but patients are not necessarily dying and can pursue curative treatments.
Traditionally, palliative care has been employed to help cancer patients in the hospital. But its practitioners are recognizing that other types of patients can benefit, too — especially those with kidney failure. The palliative care team can help patients assess whether to start or stop dialysis, and can manage the symptoms in whatever path the patient chooses.
In Burgoyne’s case, the team — doctor, nurse practitioner, social worker, and chaplain — weighed Burgoyne’s prognosis and talked with Tucker about what he thought was best for her. Did it make sense to keep doing dialysis?
“Many patients who have started dialysis, they do wonder about their prognosis. They want to talk about end of life,” said Dr. Jane Schell, professor at the University of Pittsburgh School of Medicine and one of very few doctors who specialize in both palliative care and nephrology. “We’re not asking them. We’re not inviting that conversation.”
Nephrologists and palliative care specialists are both starting to step up. Schell has noticed that many nephrologists-in-training are now making a point of acquiring palliative care skills, and medical educators are recognizing its importance.
And in Boston, the Brigham plans to start an outpatient palliative care program specifically for kidney patients. It will be one of only a handful in the country, said Tulsky, the palliative care chief.
Companies that run dialysis clinics are also getting involved.Dialysis Clinic Inc., a national nonprofit provider, has undertaken six demonstration projects that enlist help from palliative care and hospice practitioners. These programs emphasize educating patients early about their illness and their options, before a crisis. The options can include transplantation or learning to dialyze at home.
The 92-year-old Burgoyne, frail and confused, was not a candidate for either options.
Burgoyne had been the “live wire” aunt in a big family. Divorced and childless, she baby-sat her eight nieces and nephews, and then years later took care of their children. As Tucker weighed the decision, he kept in touch with his siblings and cousins.
Tucker spoke often with the care team, particularly with her attending physician, Dr. Natalya Vorontsova. “She’d say, ‘There’s no easy to this. There’s only hard,’ ” he recalled.
Finally, he made the hard decision. Tucker told his aunt she would have one more dialysis session and the restraints could come off. She was delighted.
Tucker made arrangements to move Burgoyne into a hospice service at a nursing home in Westwood. Few kidney patients get to take full advantage of hospice, because in most cases Medicare does not cover hospice when the patient is on dialysis. And when the patient stops dialysis, death typically comes in about a week.
It’s a gentle death. The patient becomes groggy, falls asleep, and doesn’t wake up.
Tucker told his relatives that now was the time to say goodbye. She had just a few days.
But Burgoyne was in no rush. She loved the new facility, Clark House at Fox Hill Village, and lingered happily for a month. In early July, three months after her fall, the hospice called to say that the end was near. Tucker, his wife, and his sister came to her side. They held her hand for her final hours.
“It was very sad,” Tucker said.
But it was peaceful, for Burgoyne — and for Tucker, too, who knew he’d made the right decision. Reflecting on it nearly a year later, he said, “At the end, I felt OK.”
From Nature.com, by Ellen F. Carney
PMM2 mutation causes PKD and hyperinsulinism
Researchers have identified a previously undescribed genetic disorder that presents with hyperinsulinaemic hypoglycaemia (HI) and polycystic kidney disease (PKD) in childhood (HIPKD). They report that this disease is caused by a promoter mutation in PMM2, which encodes the N-glycosylation enzyme phosphomannomutase 2.
In those days, she was often confused and would try to rip out the tube in her chest, implanted to enable dialysis. But her words and grimaces left no doubt that she could not bear the restraints, or her complete dependence — a life so different from what she had known just weeks earlier.
Burgoyne had chosen her nephew and his wife, Robert and Nancy Tucker, to make health care decisions if she could not. Now, her nephew spent hours at her side, distraught over her misery, anguished by the choice before him. Her hands could be freed if dialysis stopped. But dialysis was keeping her alive.
She was among the growing number of very old and very sick people who end up on dialysis, a procedure that filters toxins and other substances from the blood.
But as more elderly people suffer kidney failure, new data reveal a troubling pattern for dialysis patients: A high percentage die anyway, and even those who live longer often don’t live well. That has led some patients and doctors to consider what once might have been unthinkable: disconnecting the dialysis machine.
“We used to think, ‘Dialysis, it’s great. You get more life. You get more days. Let’s do it,’ ” said Jody Comart, director of palliative care for Hebrew SeniorLife, a Greater Boston nonprofit that provides an array of services to aging patients. “But now we understand, ‘Well, you get more days. But three days [a week] are taken up by dialysis and exhaustion and feeling crummy and you are likely to have several hospitalizations each year due to complications.’ ”
Dr. Ernest Mandel, medical director of nephrology and dialysis at Hebrew SeniorLife, said that too often dialysis is the default response to kidney failure, occurring without discussion. Patients have no idea what they’re getting into — or that they could choose another route.
Most cases of kidney failure in this country are caused by diabetes and hypertension, conditions that erode kidney function gradually over many years. Burgoyne’s illness was more sudden.
Alone in her apartment in a Foxborough senior housing project, she fell one night about a year ago. By the time a neighbor found her, she had been lying on the floor for a day or two. During those long hours without food or water, her muscles broke down and released toxins that damaged her kidneys.
She was admitted to a hospital intensive care unit, bruised and disoriented. As so often happens, Burgoyne started dialysis in a crisis — doctors call it “crashing into dialysis.” There was hope it would be temporary, that her kidneys might revive.
After a couple of weeks in the hospital, Burgoyne was admitted to the medical acute care unit at Hebrew SeniorLife, which takes care of people too sick for a nursing home but not needing a full-service hospital. Although she’d been living independently, she had a heart pacemaker, chronic obstructive lung disease, and high blood pressure, among other ailments, said Anne Carr, a nurse practitioner who cared for her at HebrewLife.
As the weeks went by, the hope for improvement waned. “We didn’t know if there was a recovery in her future,” Carr said.
Burgoyne’s wrists were tied to the bed rails all the time, because she was in danger of ripping out the permanent catheter needed for her three-times-a-week dialysis.
Tucker talked to his aunt about ending dialysis. “Do you understand what it means if we stop this? This is what is keeping you alive.” She responded with a kind of shrug, which he took to mean, “It is what it is, nothing I can do.”
In 2014, some 420,000 Americans were on dialysis at any given time, and that number has almost surely increased. Those older than 75 are the fastest-growing group of dialysis patients. Medicare spends about $88,000 annually per patient for dialysis and related services.
Dialysis has long been considered a necessary response to kidney failure, a life-saving and life-prolonging procedure. The patient’s blood is passed through a machine that removes electrolytes, toxins, and excess fluid. Younger people who are otherwise healthy can have full lives and even hold jobs while on dialysis.
Although the dialysis machine filters the blood, it doesn’t do as good a job as real kidneys. It often doesn’t even relieve the symptoms of kidney failure, which can include nausea, shortness of breath, muscle cramps, itching, tiredness, and lack of appetite. In many, dialysis induces a bone-deep fatigue. Patients also have to travel to a clinic three times a week, and spend three or four hours hooked to the machine.
To make matters worse, older people and people with multiple illnesses are prone to infections, clots, and other problems that can lead to repeat hospitalizations. Often, their health declines, and they lose the ability to manage daily activities such as bathing.
No wonder surveys have found that a majority of patients on dialysis regret starting it.
Dr. James A. Tulsky, chief of the division of palliative medicine at Brigham and Women’s Hospital, said he worries many dialysis patients would choose otherwise, if they were better informed at the outset.
“The typical answer is, ‘What else can I do?’ The answer is, there might be other options . . . and if you don’t like it, you may have the option to stop it,” he said.
A 2012 study of patients with end-stage kidney disease found that those who underwent dialysis lived 404 days longer than those who decided against the procedure. But 326 of those extra days were spent undergoing dialysis, and an uncounted number were lost to hospitalization.
Notably, for those older than 75, dialysis does not always result in any additional days of life. Studies in the Netherlands and the United Kingdom have shown that elderly patients who forgo dialysis often live about as long as those who choose the procedure.
American kidney doctors — known as nephrologists — need to change their approach, said Mandel, the Hebrew SeniorLife nephrologist. “We tended to wash our hands of the patient if they didn’t want dialysis,” he said.
Instead, he said, the decision should not be a matter of accepting or rejecting dialysis but choosing among transplantation, dialysis, or what is known as “conservative management” — a method of treating kidney disease focused on relieving symptoms and adjusting medications and lifestyle to preserve kidney function.
And then, he added, patients need to have continuing conversations about whether to change course. Stopping dialysis can be a weighty decision. Patients whose kidneys have become dependent on dialysis die quickly when it is withdrawn, within seven or eight days on average.
Although dialysis is expensive, the question of whether conservative management saves money has not been adequately studied. In any case, Mandel said, the main point is to improve patients’ quality of life.
Mandel thinks the decision to put Burgoyne on dialysis after her fall was reasonable, given the severity of her kidney failure and the hope for recovery. But, he said, she might have benefited from a conversation about what dialysis would entail and when to consider stopping it.
Once she was admitted to Hebrew SeniorLife, Burgoyne and her nephew had a chance for many conversations about her options. They were offered a service that few kidney patients get — palliative care, a team-based approach to managing serious illness that focuses on quality of life.
Palliative care is similar to hospice in that it works to treat symptoms and keep patients comfortable, but patients are not necessarily dying and can pursue curative treatments.
Traditionally, palliative care has been employed to help cancer patients in the hospital. But its practitioners are recognizing that other types of patients can benefit, too — especially those with kidney failure. The palliative care team can help patients assess whether to start or stop dialysis, and can manage the symptoms in whatever path the patient chooses.
In Burgoyne’s case, the team — doctor, nurse practitioner, social worker, and chaplain — weighed Burgoyne’s prognosis and talked with Tucker about what he thought was best for her. Did it make sense to keep doing dialysis?
“Many patients who have started dialysis, they do wonder about their prognosis. They want to talk about end of life,” said Dr. Jane Schell, professor at the University of Pittsburgh School of Medicine and one of very few doctors who specialize in both palliative care and nephrology. “We’re not asking them. We’re not inviting that conversation.”
Nephrologists and palliative care specialists are both starting to step up. Schell has noticed that many nephrologists-in-training are now making a point of acquiring palliative care skills, and medical educators are recognizing its importance.
And in Boston, the Brigham plans to start an outpatient palliative care program specifically for kidney patients. It will be one of only a handful in the country, said Tulsky, the palliative care chief.
Companies that run dialysis clinics are also getting involved.Dialysis Clinic Inc., a national nonprofit provider, has undertaken six demonstration projects that enlist help from palliative care and hospice practitioners. These programs emphasize educating patients early about their illness and their options, before a crisis. The options can include transplantation or learning to dialyze at home.
The 92-year-old Burgoyne, frail and confused, was not a candidate for either options.
Burgoyne had been the “live wire” aunt in a big family. Divorced and childless, she baby-sat her eight nieces and nephews, and then years later took care of their children. As Tucker weighed the decision, he kept in touch with his siblings and cousins.
Tucker spoke often with the care team, particularly with her attending physician, Dr. Natalya Vorontsova. “She’d say, ‘There’s no easy to this. There’s only hard,’ ” he recalled.
Finally, he made the hard decision. Tucker told his aunt she would have one more dialysis session and the restraints could come off. She was delighted.
Tucker made arrangements to move Burgoyne into a hospice service at a nursing home in Westwood. Few kidney patients get to take full advantage of hospice, because in most cases Medicare does not cover hospice when the patient is on dialysis. And when the patient stops dialysis, death typically comes in about a week.
It’s a gentle death. The patient becomes groggy, falls asleep, and doesn’t wake up.
Tucker told his relatives that now was the time to say goodbye. She had just a few days.
But Burgoyne was in no rush. She loved the new facility, Clark House at Fox Hill Village, and lingered happily for a month. In early July, three months after her fall, the hospice called to say that the end was near. Tucker, his wife, and his sister came to her side. They held her hand for her final hours.
“It was very sad,” Tucker said.
But it was peaceful, for Burgoyne — and for Tucker, too, who knew he’d made the right decision. Reflecting on it nearly a year later, he said, “At the end, I felt OK.”
PKD Research