From Business Wire, Invitation to Pre-Register for Briefing
Otsuka to Host Web Briefing on Tolvaptan Phase 3 Trial Results in Polycystic Kidney Disease
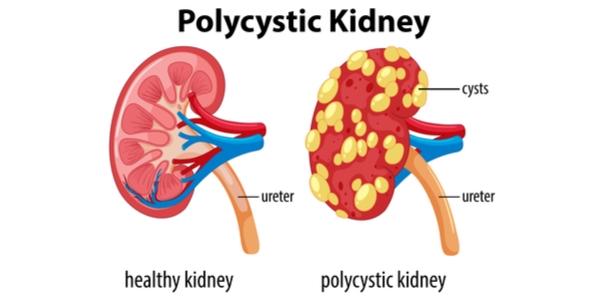
TOKYO & PRINCETON, N.J.--(BUSINESS WIRE)--Otsuka Pharmaceutical Co., Ltd. (OPCJ) and its affiliate Otsuka Pharmaceutical Development & Commercialization, Inc. (OPDC) are pleased to invite investors and media to a November 4 web briefing on in-depth results from the REPRISE phase 3 trial for tolvaptan, a drug candidate for the treatment of patients in the U.S. with autosomal dominant polycystic kidney disease (ADPKD).
To participate in the web briefing, kindly pre-register at:
http://event.on24.com/wcc/r/1534382-1/77E66445B009CE3491DBB035504DCF69
Confirmation of registration and information on how to access the web briefing on November 4 will be sent to registrants by email.
An archived version of the webcast will be accessible on the website of Otsuka Pharmaceutical Company’s parent company, Otsuka Holdings Co., Ltd., within 24 hours after the web briefing.
The REPRISE phase 3 trial data will also be presented earlier in the day on November 4 in a late breaking oral abstract session at American Society of Nephrology (ASN) Kidney Week 2017, in New Orleans (Abstract# SA-OR128). Attendees of Kidney Week 2017 are invited to attend the session, between 10:30 AM and 12:30 PM in Hall J.
The REPRISE trial was completed to supply confirmatory data to the previous studyi to address the Complete Response Letter issued by the U.S. FDA in 2013 for a New Drug Application for tolvaptan in the treatment of adults with ADPKD.
About Tolvaptan
Tolvaptan is a selective vasopressin V2-receptor antagonist. By selectively blocking vasopressin at the V2-receptor, tolvaptan has been shown to decrease cyst-cell proliferation and fluid secretion in subjects with ADPKD, ultimately reducing cyst development.iiIn a previous Phase 3 clinical trial, tolvaptan was associated with reduced kidney growth and slowed decline of kidney function.i
From Dove Medical Press, by: Satoru Muto,1 Tadashi Okada,2 Moriyoshi Yasuda,3 Hidetsugu Tsubouchi,4 Koji Nakajima,4 Shigeo Horie1,5
Long-term safety profile of tolvaptan in autosomal dominant polycystic kidney disease patients: TEMPO Extension Japan Trial
1Department of Advanced Informatics for Genetic Disease, Juntendo University Graduate School of Medicine, Tokyo, 2Department of Clinical Development, 3Pharmacovigilance Department, 4Department of Medical Affairs, Otsuka Pharmaceutical Co, Ltd, 5Department of Urology, Juntendo University Graduate School of Medicine, Tokyo, Japan
Aim: The aim of this trial (ClinicalTrials.gov identifier: NCT01280721) was to investigate the long-term safety profile of tolvaptan in Japanese patients with autosomal dominant polycystic kidney disease (ADPKD).
Aim: The aim of this trial (ClinicalTrials.gov identifier: NCT01280721) was to investigate the long-term safety profile of tolvaptan in Japanese patients with autosomal dominant polycystic kidney disease (ADPKD).
Methods: This open-label multicenter trial was conducted to examine adverse drug reactions (ADRs) related to tolvaptan up to an additional 3 years in 135 Japanese patients who participated in the Tolvaptan Efficacy and Safety in Management of Autosomal Dominant Polycystic Kidney Disease and its Outcomes (TEMPO) 3:4 trial at doses of 60–120 mg/d. Blood samples were collected at baseline; at weeks 1, 2, and 3; at month 3; and every 3 months thereafter.
Results: In total, 134/135 (>99%) patients experienced ADRs. The most frequent ADRs were thirst (77.0%), pollakiuria (57.0%), polyuria (37.8%), and hyperuricemia (14.8%). Any unexpected ADRs were not reported in this trial. Most ADRs occurred early during treatment. Fourteen patients (10.4%) experienced hepatic events, and 8 (5.9%) experienced >3-fold increases above the upper limits of normal in serum alanine aminotransferase or aspartate aminotransferase levels between 3 and 9 months following tolvaptan initiation, which recovered after drug interruption. Of the 8 patients, 7 (5.2%) were previously allocated to the placebo arm in the TEMPO 3:4 trial and 4 (3.0%) discontinued due to the hepatic events. One patient (0.7%) was previously allocated to tolvaptan and experienced similar events in the TEMPO 3:4 trial. None of the hepatic ADRs met Hy’s Law laboratory criteria.
Conclusion: ADRs observed in this extension trial were similar to those identified in the TEMPO 3:4 trial and hepatic events were not progressive.
From News-Medical
A new study finds that kidney transplantation prolongs the lives of not only patients who have recently initiated dialysis, but also those who have been undergoing dialysis for more than a decade. The findings, which appear in an upcoming issue of the Clinical Journal of the American Society of Nephrology (CJASN), indicate that patients who may not have been referred for transplantation should be reevaluated.
In individuals with kidney failure, kidney transplantation is associated with longer survival than dialysis; however, this information comes from studies during an era in which patients received transplants relatively rapidly. Today, 13% of the nearly 100,000 wait-listed kidney transplant candidates in the United States have had kidney failure for more than 11 years.
John Gill, MD, MS (University of British Columbia and Vancouver's Providence Health Care) and his colleagues examined whether patients who receive transplants after prolonged treatment with dialysis derive a similar survival benefit as those who undergo transplantation earlier. "Because of recent changes in allocation policy, patients not previously wait-listed for many years can rapidly access transplantation if they are referred for transplantation and accepted onto a waiting list. We wanted to determine if these 'forgotten' patients might still benefit from transplantation despite being treated with dialysis for a very long period of time," said Dr. Gill. The researchers suspected that the benefit might not be the same because pre-transplant dialysis exposure is associated with inferior post-transplant kidney survival.
The team's study of 5365 patients in the Scientific Registry of Transplant Recipients determined the risk of death in recipients of a deceased donor kidney transplant after 10 or more years of dialysis treatment compared with wait-listed patients who continued to undergo dialysis. Patients were followed for at least 5 years.
The overall death rate for patients who underwent transplantation was 3.9 per 100 patient-years, compared with 5.8 per 100 person-years for patients who continued on dialysis. (A person-year is the number of years of follow-up multiplied by the number of people in the study.) After adjustments, transplant recipients had a 40% lower risk of dying than patients on dialysis who had equal lengths of follow-up from their 10-year dialysis anniversary. This benefit was observed in a variety of patient sub-groups, including patients ≥65 years of age and patients with diabetes. Transplant recipients were at higher risk of death for 180 days after transplantation, however, and they did not derive survival benefit until 657 days after transplantation, despite receiving good quality kidneys.
"Because transplantation is associated with longer survival in patients who have more than 10 years of dialysis treatment, patients who might not have been referred for transplantation should be reevaluated, as they might benefit," said Dr. Gill.
MENTOR Results, New Trial Design Pitches at Kidney Week
NEW ORLEANS — Results from the MENTOR trial, a randomized comparison of rituximab and cyclosporine for the treatment of membranous nephropathy, will be in the spotlight here at Kidney Week 2017.
The noninferiority study looked at the long-term remission of proteinuria in patients with this challenging disease.
Also of interest will be a pragmatic clinical trial demonstration project from the National Institutes of Health, said Patrick Nachman, MD, from the University of North Carolina Kidney Center in Chapel Hill, who is chair of the ASN postgraduate education committee.
The "results may give us an idea of how we can think about clinical trials differently than the traditional randomized trial, which of course has benefits, but also some limitations," he told Medscape Medical News.
During the high-impact clinical trials session, studies will be presented on a new candidate molecule for the prevention of acute kidney injury after cardiac surgery; the use of ultrasound-guided percutaneous arteriovenous fistula to improve hemodialysis access; and whether or not tolvaptan (Samsca, Otsuka Pharmaceutical), a vasopressin receptor 2 antagonist, can slow the inevitable decline in kidney function in patients with later-stage autosomal dominant polycystic kidney disease.
And new analyses of data from big name clinical trials — such as the EMPA-REG OUTCOME trial and the Peritoneal Dialysis Outcomes and Practice Patterns Study — will be presented.
The effective prevention of kidney injury after the use of either intravenous or intracoronary contrast agents during coronary angiography will be addressed in an industry-independent phase 3 clinical trial.
In individuals with kidney failure, kidney transplantation is associated with longer survival than dialysis; however, this information comes from studies during an era in which patients received transplants relatively rapidly. Today, 13% of the nearly 100,000 wait-listed kidney transplant candidates in the United States have had kidney failure for more than 11 years.
John Gill, MD, MS (University of British Columbia and Vancouver's Providence Health Care) and his colleagues examined whether patients who receive transplants after prolonged treatment with dialysis derive a similar survival benefit as those who undergo transplantation earlier. "Because of recent changes in allocation policy, patients not previously wait-listed for many years can rapidly access transplantation if they are referred for transplantation and accepted onto a waiting list. We wanted to determine if these 'forgotten' patients might still benefit from transplantation despite being treated with dialysis for a very long period of time," said Dr. Gill. The researchers suspected that the benefit might not be the same because pre-transplant dialysis exposure is associated with inferior post-transplant kidney survival.
The team's study of 5365 patients in the Scientific Registry of Transplant Recipients determined the risk of death in recipients of a deceased donor kidney transplant after 10 or more years of dialysis treatment compared with wait-listed patients who continued to undergo dialysis. Patients were followed for at least 5 years.
The overall death rate for patients who underwent transplantation was 3.9 per 100 patient-years, compared with 5.8 per 100 person-years for patients who continued on dialysis. (A person-year is the number of years of follow-up multiplied by the number of people in the study.) After adjustments, transplant recipients had a 40% lower risk of dying than patients on dialysis who had equal lengths of follow-up from their 10-year dialysis anniversary. This benefit was observed in a variety of patient sub-groups, including patients ≥65 years of age and patients with diabetes. Transplant recipients were at higher risk of death for 180 days after transplantation, however, and they did not derive survival benefit until 657 days after transplantation, despite receiving good quality kidneys.
"Because transplantation is associated with longer survival in patients who have more than 10 years of dialysis treatment, patients who might not have been referred for transplantation should be reevaluated, as they might benefit," said Dr. Gill.
From MedScape, by Pam Harrison
NEW ORLEANS — Results from the MENTOR trial, a randomized comparison of rituximab and cyclosporine for the treatment of membranous nephropathy, will be in the spotlight here at Kidney Week 2017.
The noninferiority study looked at the long-term remission of proteinuria in patients with this challenging disease.
Also of interest will be a pragmatic clinical trial demonstration project from the National Institutes of Health, said Patrick Nachman, MD, from the University of North Carolina Kidney Center in Chapel Hill, who is chair of the ASN postgraduate education committee.
The "results may give us an idea of how we can think about clinical trials differently than the traditional randomized trial, which of course has benefits, but also some limitations," he told Medscape Medical News.
During the high-impact clinical trials session, studies will be presented on a new candidate molecule for the prevention of acute kidney injury after cardiac surgery; the use of ultrasound-guided percutaneous arteriovenous fistula to improve hemodialysis access; and whether or not tolvaptan (Samsca, Otsuka Pharmaceutical), a vasopressin receptor 2 antagonist, can slow the inevitable decline in kidney function in patients with later-stage autosomal dominant polycystic kidney disease.
And new analyses of data from big name clinical trials — such as the EMPA-REG OUTCOME trial and the Peritoneal Dialysis Outcomes and Practice Patterns Study — will be presented.
The effective prevention of kidney injury after the use of either intravenous or intracoronary contrast agents during coronary angiography will be addressed in an industry-independent phase 3 clinical trial.