From BMC Nephrology
Background
Autosomal dominant polycystic kidney disease (ADPKD) accounts for 8–10% of end-stage chronic kidney disease (CKD) patients worldwide. In the last decade, the advanced knowledge in genetics and molecular pathobiology of ADPKD focused some aberrant molecular pathways involved in the pathogenesis of the disease leading to controlled clinical trials aimed to delay its progression with the use of mTOR inhibitors, somatostatin or tolvaptan. Preclinical studies suggests an effective role of metformin in ADPKD treatment by activating AMPK sensor. Clinical trials are currently recruiting participants to test the metformin use in ADPKD patients.
Methods
We retrospectively examined the records of our ADPKD patients, selecting 7 diabetic ADPKD patients under metformin treatment and 7 matched non-diabetic ADPKD controls, to test the effect of metformin on renal progression during a 3 year follow-up.
Results
During the first year, the GFR decreased by 2.5% in Metformin Group and by 16% in Controls; thereafter, renal function remained stable in Metformin Group and further decreased in Controls, reaching a 50% difference after 3 years of observation. Accordingly, the overall crude loss of GFR, estimated by a linear mixed model, resulted slower in the Metformin than in Control Group (− 0.9; 95% C.I.: -2.7 to 0.9 vs - 5.0; 95% C.I.: -6.8 to − 3.2 mL/min/1.73 m2 per year, p = 0.002).
Conclusions
Our data are suggestive of a beneficial effect of metformin on progression of ADPKD. Large, randomized, prospective trials are needed to confirm this hypothesis.
From PharmiWeb, Press Release
Research in Polycystic Kidney Disease Takes an Important Step Forward Sanofi begins pivotal clinical trial to evaluate therapy for patients at risk of rapidly progressing autosomal dominant polycystic kidney disease (ADPKD)
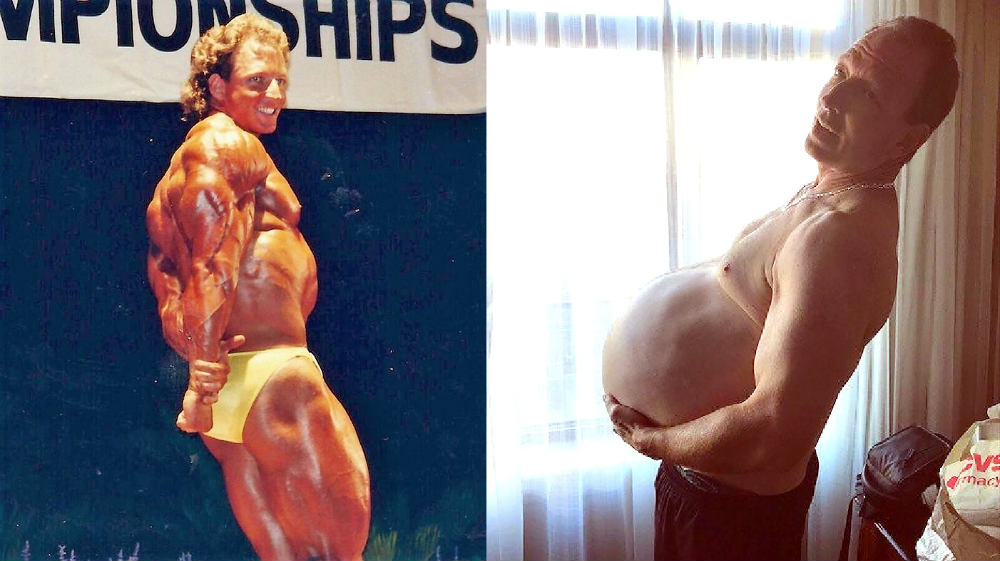
BRIDGEWATER, N.J., Oct. 26, 2018 /PRNewswire/ -- Autosomal dominant polycystic kidney disease (ADPKD) is a devastating rare genetic kidney condition that leads to the growth of numerous cysts in the kidneys. Affecting an estimated 120,000 people in the U.S. and 170,000 in the European Union, ADPKD becomes so severe for approximately half of those patients that they face either a lifetime of dialysis or a kidney transplant.
Sanofi is beginning a pivotal clinical trial to study the safety, efficacy, and tolerability of an investigational oral agent called venglustat for certain patients with ADPKD. The international trial is enrolling patients who are at risk of rapidly progressive ADPKD.
"The initiation of this clinical trial is another reflection of Sanofi's commitment to research, advanced scientific discovery, and true innovation," said Gianluca Pirozzi, Head of Development for Rare Diseases and Head of Translational Gene Therapy, Sanofi Genzyme, the specialty care global business unit of Sanofi. "Our understanding thus far of both the cause and progression of ADPKD and the mechanism of action of venglustat present us with a path forward in this research effort."
Genetic mutation leads to devastating condition
ADPKD is caused by a mutation in the PKD1 or PKD2 gene that leads to a build-up of complex substances called glycosphingolipids in the kidneys. Glycosphingolipid accumulation is thought to be an important driver of cyst growth1,2. Relentless cyst growth can cause chronic pain and lead to reduced kidney function and kidney failure in ADPKD patients. The symptoms of ADPKD usually start to appear between the ages of 30 and 40, but they can begin as early as childhood for some patients.3
"The PKD Foundation welcomes research efforts that have the potential to bring new therapies to patients living with this condition," said David Baron, Ph.D., Chief Scientific Officer of the PKD Foundation. "We appreciate that Sanofi has engaged with the ADPKD patient community throughout the early stages of clinical development for venglustat and look forward to continuing to work with Sanofi."
About Venglustat
Venglustat is an investigational oral therapy designed to inhibit the abnormal accumulation of a substance in the body called glucosylceramide (GL-1), which plays a role in production of glycosphingolipids. In genetic mouse models of ADPKD, inhibition of glycosphingolipid production has been shown to reduce kidney cyst growth.4 The clinical significance of this is under investigation.
"Venglustat represents a potential opportunity for Sanofi Genzyme to expand its core legacy of expertise in lysosomal storage disorders and make an impact on patients living with other rare and challenging diseases," said Sébastien Martel, Global Head of Rare Diseases, Sanofi Genzyme. "Our progress related to evaluating venglustat in ADPKD once again highlights our company-wide commitment to continually build on our experience and focus our research efforts on unmet needs for patients around the world."
Venglustat has received Orphan Drug designation in the U.S. for the treatment of ADPKD. The ADPKD clinical trial will be conducted at sites in the U.S., Canada, China and Japan as well as several EU countries.
For more information on this trial, please visit https://www.clinicaltrials.gov or https://www.clinicaltrialsregister.eu. U.S. patients interested in learning more, may also visit https://adpkdtrial.org.
From Global News Wire, Press Release
● Shorter Path to XRx-008 Marketing Approval ●
XORTX Therapeutics Inc. ("XORTX" or the “Company”) (CSE:XRX; OTCQB:XRTXF), a biopharmaceutical company focused on developing innovative therapies to treat progressive kidney disease (“PKD”), is pleased to announce that the Company’s clinical development plan has been reviewed and accelerated. This major revision to the Company’s original clinical development plan was acceptable to the US Food and Drug Administration (“FDA”) subsequent to XORTX’s submission of its pre-Investigational new drug (“IND”) information package and the Company’s in-person meeting held September 20, 2018 to discuss the comprehensive development plan.
Discussions with the FDA ranged across developmental topics including manufacturing, formulation, non-clinical study plans and clinical development strategy for XRx-008, including:
Review of XORTX’s proposed chemistry, manufacturing and formulation was confirmed by the FDA as acceptable with no material changes;
The proposed non-clinical development proposal was reviewed and confirmed the importance of characterizing the scale of increased bioavailability of XRx-008 in advance of clinical study initiation;
The proposed clinical development program for XRx-008, as a therapy for patients with PKD was outlined by the XORTX team and was composed of separate phase 2 and phase 3 clinical trials, followed by marketing application (NDA). Discussion and exploration with the FDA suggested a substantially shorter path to marketing approval for XRx-008 for ADPKD; and
The outcome of the pre-IND meeting is an accelerated clinical development plan composed of a study to characterize bioavailability XRx-008 in man, then a single, pivotal phase 2/3 clinical trial which would be eligible for special protocol assessment (SPA – see further information below).
Dr. Allen Davidoff, XORTX’s CEO stated, “We are very pleased with the positive meeting we had with the FDA that clarified that XORTX can simplify and accelerate its clinical study plan. The Company has now defined four clear steps to develop XRx-008 for autosomal dominant polycystic kidney disease patients (“ADPKD”): (i) manufacture clinical study ready drug for our upcoming clinical trials; (ii) file the IND and characterize the bioavailability and pharmacokinetics of XRx-008 in humans; (iii) complete the orphan drug designation (“ODD”) process for this program (see further information below); and, (iv) complete a pivotal phase 2/3 clinical trial. XORTX will seek a special protocol assessment (SPA) for this pivotal study. This accelerated clinical development plan substantially decreases the time and cost to bring this therapy to patients with PKD.”
Special Protocol Assessment (“SPA”) is one optional type of agreement submission that is available to sponsors, such as XORTX, for pivotal phase 3 trials. Through the SPA process, the sponsor and the FDA negotiate the design of a clinical trial that will support an efficacy claim for marketing approval. One advantage of the SPA is that, if an agreement is reached, XORTX would then have clarity in writing of the endpoints that must be achieved to support marketing approval.
Orphan Drug programs in the United States are programs for the treatment of rare disease which were passed into law in 1983 to facilitate development of orphan drugs – drugs for rare diseases such as ADPKD, Huntington’s disease, ALS and muscular dystrophy. These rare diseases typically have fewer than 200,000 patients living in the US and due to small patient numbers would not be considered economically feasible without government programs to support their economic viability. ODD does not indicate that the therapeutic is either safe and effective or legal to manufacture and market in the United States. That process is handled through other offices in the FDA, however an ODD designation would qualify XORTX for a number of benefits from the US federal government, such as reduced taxes and grants to fund future clinical trial work – a potentially substantial non-dilutive funding benefit to shareholders. Similar programs for rare diseases exist in European Union, Japan and other countries. Orphan drugs generally follow the same regulatory development path as any other pharmaceutical product, in which testing focuses on pharmacokinetics and pharmacodynamics, dosing, stability, safety and efficacy, however, some statistical burdens are lessened in an effort to maintain development momentum. As a result of world wide support for the development of therapeutic solutions to disease, orphan programs are some of the most successful, time and cost effective programs to develop.