From The Press and Journal, Aberdeen, United Kingdom, by Davis Kerr
Man forced to wait four years for kidney transplant

An Orkney man has criticised the Scottish Government after being forced to wait for years for a new kidney.
Steve Sankey spent four years waiting for and organ transplant and had to endure three years of dialysis and regular flights to Aberdeen for check-ups.
But he believes he and others in his situation could be spared the wait if the government adopted an “opt out” system for organ donations.
At present people have to sign up to the organ donor register for their organs to be used in transplants.
The government said it was committed to increasing the number of donors but evidence was split on whether an opt-out system would work.
Mr Sankey had been living with adult polycystic kidney disease, which left him with only 5% of organ function and meant he had to undergo dialysis.
The 59-year-old wildlife guide finally received a new kidney on Tuesday, September 15 at Edinburgh Royal Infirmary.
He said “Naturally I’m delighted with my new kidney, which after a month is working well and thus far all appears to be fine.
“The medics are really pleased with progress, as are all my family and friends. I had great support from everyone, especially down in Edinburgh, where I used to work, and I’d like to pay tribute to the professionalism of the transplant team in Edinburgh and the renal team in Aberdeen.”
Mr Sankey recently travelled to the Scottish Parliament for the launch of a private member’s bill being led by Labour MSP Anne McTaggart to try to change the law on organ donation.
He said: “It’s hugely disappointing that the Scottish Government has chosen not to include this piece of legislation in their programme – it could help so many others in my predicament.
“Instead we’re having to rely on a private member’s bill to try and get the organ donation system into a ‘soft opt-out’ one like many other European countries, including Wales.
“If I had been a resident of Spain, for example, I would have probably had a transplant several years ago, as the supply of organs through the different system is much greater than in the UK.”
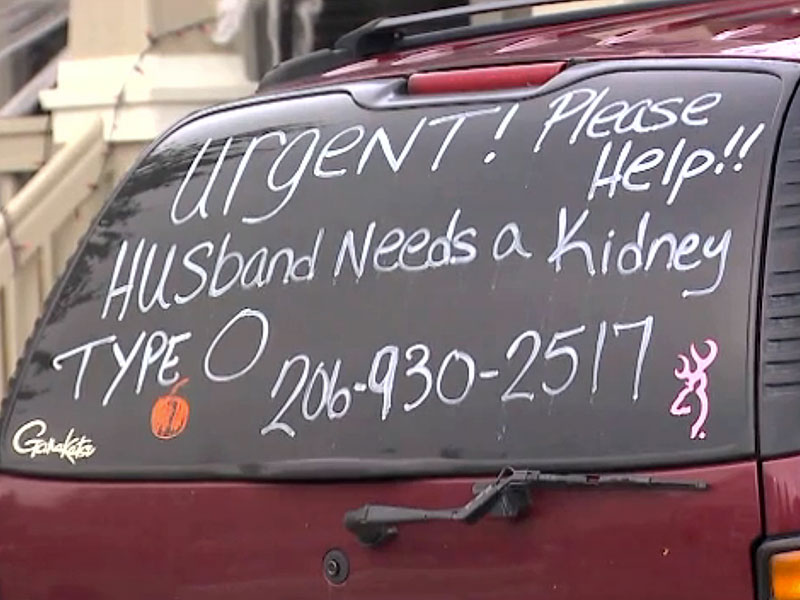
"Urgent!" reads a messagein large letters on her family's car. "Please help!! Husband needs a kidney. 206-930-2517."
Amy's husband, 57-year-old Sorin Malancioiu, needs a kidney, and it could take as long as six years for him to receive one through the organ transplant waiting list as his type O blood is the most difficult to match, KOMO newsreports.
Sorin suffers from an inherited disorder called Polycystic Kidney Disease, his wife explained on GoFundMe. The disease caused cysts to grow on the father of two's kidneys until they became too compromised to function and were removed in 2014.
"Just seven years ago, Sorin led a very active lifestyle," Amy wrote. "Since the surgery this past June, he has been on dialysis 3 days a week for 4 hours a day. He is exhausted, listless and in pain after each session."
Faced with six more years of these painful treatments and uncertainty about the future, Amy decided to take matters into her own hands.
"I don't want to wait for [a kidney] to come to us," Amy told the news station. "I want to go out and get it."
Amy, one of the couple's daughters and a close family friend are driving around with the plea written on their car windows.
"It's amazing the response I'm getting," Amy said. "It's time to spread the word as fast as we can hoping that somebody would be willing to donate – to get him a kidney faster so he doesn't have to live like he does now."
The couple said they've received 20 serious offers from people who say they're willing to donate. Finding a match will still be extremely difficult as donors must have type O blood, be non-smokers, over 21 years old and in good health.
Still, they remain hopeful their unusual tactic will yield results.
"I believe this could lead to a donor, to the right person," Sorin said.
Until it does, Amy will continue the search.
"It's just incredible to have somebody like her," Sorin said. "I'm the luckiest man. I am so lucky to have such a wonderful marriage."
CALGARY – A Calgary woman who has suffered from polycystic kidney disease for 15 years posted her plea for a donor on Facebook in June, writing, “the only way I will get a kidney before I die is to find one on my own and social media will be the best way.”
She was right.
“I wrote it and I shared it to a friend, and that friend, Linda, shared it to everybody,” said Lynne Prodaniuk, who has been on the donor list since 2007 with three attempted matches, but no success.
She said she nearly died in 2000 as doctors weren’t initially sure what was wrong. At one point in her treatment, her kidney function fell to 12 per cent. She said she had a catheter put in her abdomen to start dialysis, but by 2014, the dialysis was no longer cleaning her blood well enough, and her toxicity levels increased. She said she had surgery and started hemodialysis in hospital, and has been going for eight-hour treatments since then.
Prodaniuk said when she joined the donor list, the wait was estimated between four and six years. When she got to six years, she was told the wait time had increased to eight years. She passed her seven-year anniversary July 26.
Then, another friend’s Facebook post turned things around for Prodaniuk.
“I posted on Facebook that I needed a handyman, a window company recommendation, and a kidney,” Erin Kelly told Global News.
“Mostly I was kidding about the kidney but I put it out there anyway because my Facebook friends are awesome and I was secretly hoping someone would at least inquire.”
Kelly’s friend, Shamus Neeson, replied right away. Neeson works for Canadian Blood Services and has donated blood many times, so he was curious about the living donor process.
“It was something that I felt that I should look into, if I could help save someone’s life…it just made sense,” said Neeson. “I put a call in to the living donor program, they sent me a package of very basic screening questions on my family history and what not and then we just started going from there.”
Neeson has now gone through all required kidney and cardiovascular testing and been given the go-ahead. The two new friends are waiting for the green light from Alberta’s living donor program, and from there will schedule surgery.
“I can’t believe that somebody would want to do that for a stranger,” Prodaniuk said of Neeson’s generosity, but he said it was “easy.”
“I was surprised at how easy this whole process has been,” he said. “I know that I’ve talked about how much medical testing you have to go through [but] it’s been so easy. I’m surprised more people don’t do it.”
“I always believe that we’re here to help each other.”
READ MORE: How Albertans can become living organ donors
Prodaniuk said she’s tired of “living in a prison” and can’t wait to get her life back.
“We’re going to Australia because I have a friend in Sydney and we are going to have Christmas on the beach with a barbecue.”
If you would like more information on how to become a living donor, you can contact one of Alberta’s transplant programs.
For living kidney donor services, call the Southern Alberta Transplant Program at 403-944-4635.
For information on living kidney, liver or lung donation, call the Northern Alberta Transplant Services Living Donor Program at 780-407-8698.
Dialysis News
From Senior Journal
These individuals typically have many health problems, are at higher risk of hospital readmissions, and suffer from fragmented care.
The Centers for Medicare & Medicaid Services (CMS) has announced the participants for the Comprehensive ESRD Care (CEC) Model, a new accountable care organization (ACO) model made possible by the Affordable Care Act and conducted by the CMS Innovation Center.
CMS says it is part of the Department of Health and Human Services’ approach to building a health care delivery system that results in better care while using taxpayer dollars more wisely,
ACOs are groups of physicians and other health care providers who collectively take on responsibility for the quality and cost of care for a population of patients. The CEC Model is designed specifically for beneficiaries with ESRD and builds on experiences from other models and programs with ACOs, including the Pioneer ACO Model and the Medicare Shared Savings Program.
In the CEC Model, dialysis facilities, nephrologists, and other providers have joined together to form ESRD Seamless Care Organizations (ESCOs) to coordinate care for ESRD beneficiaries. ESCOs will be financially accountable for quality outcomes and Medicare Part A and B spending, including all spending for dialysis services, for their ESRD beneficiaries.
This model will encourage dialysis providers to think beyond their traditional roles in care delivery and support beneficiaries as they provide patient-centered care that will address beneficiaries’ health needs in and out of the dialysis facility.
“This new ACO model represents a paradigm shift in care for beneficiaries with end-stage renal disease; it promotes a patient-centered approach to their dialysis and non-dialysis care needs that will help accomplish our delivery system reform goals of better care, smarter spending, and healthier people,” said Patrick Conway, M.D., MSc, acting deputy administrator and chief medical officer, CMS.
The CEC Model includes separate financial arrangements for ESCOs with large and small dialysis organizations. ESCOs with participation by a dialysis facility or facilities owned by a large dialysis organization, which is an organization that owns 200 or more dialysis facilities, will be eligible to receive shared savings payments. They will also be liable for shared losses, and will have higher overall levels of risk compared with their smaller counterparts.
ESCOs with participation by a dialysis facility or facilities owned by a small dialysis organization, which is an organization that owns fewer than 200 dialysis facilities, will be eligible to receive shared savings payments, but will not be liable for shared losses.
The CEC Model is part of the Department’s efforts to create opportunities for providers to enter into alternative payment models and meet the Secretary’s goal, announced on January 26th, to have 30% of traditional Medicare payments paid through alternative payment models by the end of 2016 and 50% by the end of 2018.
From Med Device Online, by Jof Enriquez
"PD is an important treatment option for many patients with kidney disease seeking home-based therapy," said Jaime Uribarri, M.D., Department of Nephrology, Mt. Sinai Hospital, NY, in the announcement. "We welcome new technology that allows patients to start and administer their physician-prescribed PD therapy at home."
Baxter collaborated with DEKA Research and Development Corporation (DEKA) in developing the AMIA APD system, which the company claims is the only device cleared in the U.S. that incorporates patient-centric features like voice guidance, a touchscreen control panel with animated graphics, and the SHARESOURCE two-way connectivity platform, which allows remote access by healthcare providers.
"Enabling patients to actively work with their healthcare providers to initiate and confidently manage their dialysis therapy is the ultimate goal in the development of AMIA with SHARESOURCE," said Bruce Culleton, M.D., VP, renal therapeutic area lead, Baxter, in the announcement. "Baxter's focus is to understand and support access to the best renal replacement options for all patients, and then bring technology like AMIA and SHARESOURCE to healthcare providers so they can help their patients achieve their best possible outcomes."
According to Baxter, it will launch the AMIA APD system with SHARESOURCE this year in the U.S., where some 600,000 individuals are living with end-stage renal disease (ESRD), which is treated with either hemodialysis, PD, or a kidney transplant.
Unlike hemodialysis, which draws out blood from the body to be cleansed by a dialyzer, peritoneal dialysis makes use of the abdominal lining — called the peritoneum — as a dialyzing membrane to cleanse the blood and clear excess fluid. Automated PD devices called cyclers utilize clamps to control the flow of fluids in and out of the abdomen. The machines are pre-programmed and the fluid exchanges are performed automatically while the patient sleeps.
No comments:
Post a Comment