From News-Medical.net, By Dr Liji Thomas, MD
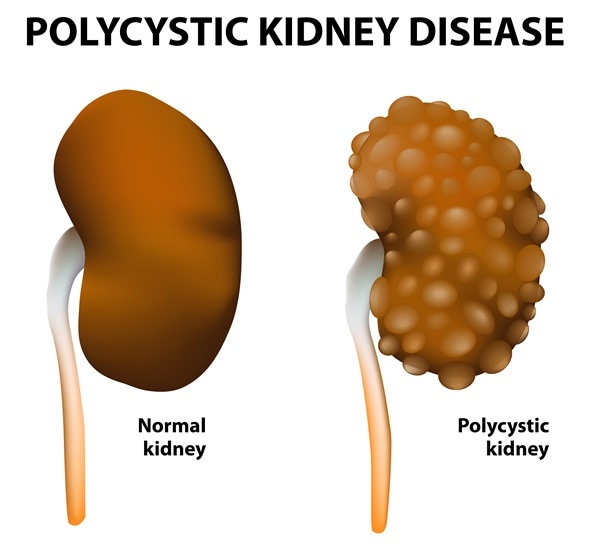
Polycystic kidney disease (PKD) is a hereditary condition in which the kidneys develop multiple cysts. This leads to renal enlargement, distortion of the normal structure of the kidneys and functional impairment.
The result may be chronic kidney disease, progressing to end-stage kidney disease (ESRD) requiring dialysis or kidney transplantation.
It affects both genders and all ethnic groups but leads to chronic kidney disease in males and in women who had three or more pregnancies and who have high blood pressure.
Symptoms
PKD often presents with pain in the back and the sides of the ribcage and headaches, while hematuria is sometimes present. In autosomal recessive PKD, enlarged kidneys, respiratory distress and growth failure in infants may be the presenting symptoms.
Incidence of PKD
PKD may be autosomal dominant or recessive. Autosomal dominant PKD occurs in up to one in 400 people but the autosomal recessive type occurs in one in 20 000 – 40 000 people.
Complications of PKD
Pain in the back or sides
Chronic renal disease
Frequent urinary tract infections
Renal failure
High blood pressure
Liver and pancreatic cysts
Abnormal heart valves
Aneurysms in the brain and heart
Intestinal diverticula
Hematuria
Kidney stones
Respiratory arrest, growth failure and hepatic dysfunction in childhood, in the autosomal recessive type
Why does PKD occur?
PKD is the result of a gene defect, which is usually present in the parent and is passed on to the offspring. At least three mutations have been found to be associated with PKD, of which two are found in the autosomal dominant type.
The most common form of PKD is the autosomal dominant type. It usually starts between 30 and 50 years, but symptoms start only when the cysts have reached a size of 0.5 cm or more. In the recessive form, cysts form in infancy or even in utero.
Diagnosis and treatment
Genetic testing is carried out on saliva or blood and looks for the presence of specific gene mutations. This helps with diagnosis as well as predicting the chances of passing on the disease. Prenatal genetic testing can identify the presence of the gene in fetuses in utero. However, genetic testing fails to predict the time of onset of symptoms or their severity.PKD is diagnosed on the basis of imaging tests and genetic testing. Imaging the kidneys involves ultrasound, CT scans or MRI scans. A scan which shows two or more cysts before the age of 30, for instance, combined with a family history of PKD, may lead to a diagnosis of the condition.
PKD has no cure and treatment is directed towards symptom control and achieving a longer life. This may involve cyst removal to relieve pain, bringing down the blood pressure, lifestyle changes and monitoring for heart valve complications or brain aneurysms. For instance, diet is important in preventing some complications, mostly due to high blood pressure and so a low-sodium diet with high intake of vegetables is often recommended, with more poultry, fish or dairy products for protein.
In the autosomal recessive form of PKD, the kidneys may be so large that they prevent normal breathing. In such cases, nephrectomy is unavoidable and such children must receive a kidney transplant or dialysis. Proper growth is ensured by dietary guidelines, sometimes in conjunction with growth hormone treatment for severe growth arrest.
Respiratory arrest is always a possibility in infants with the severe form of the disease and ventilator support is often required, as well as cardiopulmonary resuscitation in emergency situations. Kidney function is replaced by dialysis, usually peritoneal, but also hemodialysis in some cases. Control of urinary infections, hypertension and measures to slow the progression of liver disease is required. Combined liver and kidney transplantation is necessary in some cases.
PKD, Gift of Life
From Eagle Tribune, North Andover, MA, By Zoe Mathews

The sign out front of Common Grounds Cafe that once asked for a kidney donor has had its message changed from plea to praise. That's because RuthEllen "Kiki" Bernard found what she was looking for -- a matched kidney donor.
Kiki, who suffers from polycystic kidney disease, found a donor just weeks after the sign went up at the hands of her husband, Wayne. The couple said finding a donor wouldn't have happened without the sign, which brought curious passersby into the cafe to ask questions, and garnered more conversation and awareness in the community about organ donation.
The couple learned Kiki's kidneys were functioning at about 20 percent at the beginning of the year, and that she would need a kidney donor or face dialysis treatment. They kept things under wraps, not reaching out to family or friends. They faced the daunting and lengthy kidney donor waiting list alone.
"It's not something we'd talk about over dinner," said Wayne. "In a way, we didn't have to go through all of this if we had just been more open about what was going on."
But then in June, months after Kiki found out about her failing kidneys, Wayne put up the initial sign out front of his cafe on Route 97.
The sign, and the increased word of mouth, forced the couple to start talking about what was going on, and that communication extended into the Bernard family.
Lisa Twombly, Wayne's niece, had her blood drawn for compatibility testing as soon as she heard about Kiki's situation. Meanwhile, the couple said hundreds of people came through Common Grounds' doors inquiring. Not all filled out the donor applications the couple had on hand, but the couple estimates more than a dozen did.
"I said even before I knew my blood type that it was going to be me," said Twombly.
Twombly got her results last week and found out she was a near perfect match for Kiki, who scored a nine out of 100 on an antibody test that compares a transplant's recipients blood with the general population.
"I have a low antibody count, so based on 100, I have a score of nine, which means that if there were 100 donors, only nine wouldn't be a match," said Kiki.
And Twombly said her test only showed one antibody against Kiki's, meaning that the likelihood Kiki's body will accept Twombly's kidney is fairly high.
The next step for Twombly is a rigorous set of tests to ensure she is mentally and physically healthy enough to donate an organ, slated for mid-August.
When Twombly told her sons what she might be doing for her aunt, they were initially afraid for her.
"My son, Taylor, was scared about the surgery," she said of her 10 year old. "But I told him how he had surgery too, he has cochlear implants, and later he came up to me and said how he thought I was a hero, and was brave for doing this. So that feels amazing."
Just one day after the updated sign went up thanking people, Wayne said more than 20 people have come into the cafe to offer congratulations.
"There was a woman who dropped off green pins for kidney transplant recipients, like the breast cancer pins. And one daily customer, we found out got a kidney transplant 30 years ago," he said. "It's everywhere, and apparently it's just something nobody talks about."
This experience motivated Wayne to consider donating one of his own kidneys. He said he has learned so much about people suffering from kidney disease, that he's thinking about donating his kidney to start a chain -- his kidney would be transplanted into a recipient who had a donor willing to give a kidney but wasn't a match, and the incompatible donor gives a kidney to someone else.
Kiki was initially skeptical of Wayne putting the sign up; he had done it without her knowledge. But after the outpouring of support, she felt she had to let people know how grateful she was, so she put up the new sign that reads "THANK YOU - THANK YOU - WE HAVE A DONOR".
The numbers are staggering. Because of a lack of donor kidneys, an average of 13 people die every day while waiting for a transplant. There are more than 100,000 names on the kidney waiting list in the U.S. and another 30 million people with chronic kidney disease who are at risk of joining them. More than 85% of those on the waiting list in 2015 are still waiting.
The good news is that there were 17,878 kidney transplants in the U.S. last year, the most in a single year, according to the United Network for Organ Sharing. And the numbers may keep growing thanks to an innovative voucher program that started in 2014 at Ronald Reagan UCLA Medical Center and is spreading across the country.
Here’s how it works: If you donate a kidney now, you will receive a voucher that a loved one could use to secure a kidney in the future. The Advanced Donation program is coordinated through the National Kidney Registry, which uses a national database to quickly and efficiently match donors and recipients.
The idea was approved by the Ethics Committee of the American Society of Transplant Surgeons in June, and has been sent to that group’s executive committee for formal approval. Ten hospitals across the country have so far joined UCLA to honor the voucher program. Donors currently need to go to one of these hospitals to receive a voucher but many other centers are expected to join.
The voucher idea is the brainchild of retired judge Howard Broadman. His grandson Quinn was born with a single kidney that wasn’t fully functioning. The retiree knew that eventually the boy would need a lifesaving transplant. Yet Mr. Broadman, who was 60 years old when Quinn was born, knew that by the time the boy needed a kidney transplant, his grandfather would be too old to donate.
Mr. Broadman approached Ronald Reagan UCLA Medical Center and proposed a simple but brilliant idea. He offered to donate a kidney immediately to a stranger on the waiting list, if in return he could secure a kidney for his grandson when the time comes. Quinn would be prioritized for a kidney when he needed a transplant.
Nothing like this had ever been done, but the UCLA Living Donor Committee and the National Kidney Registry Medical Board agreed to do it. In December 2014, Mr. Broadman donated a kidney, and 4-year-old Quinn now has a voucher to redeem when he needs it, perhaps avoiding dialysis.
If only one-half of 1% of adults in the U.S. agreed to become living donors, we could rapidly clear the waiting list for kidneys. As dramatic as this sounds, it is important that potential donors be fully informed of the risks of donating a kidney. There is a 3 in 10,000 death rate and approximately a 5 in 1,000 chance that donors will develop end-stage renal disease.
Living-donor kidneys are ideal because they generally function twice as long as kidneys from deceased donors—indirectly reducing the wait list. Nearly 700,000 people are now on kidney dialysis in the U.S. Treating end-stage renal disease costs more than $30 billion each year—and takes an enormous physical and emotional toll on patients and their families. Imagine if doctors could address kidney disease long before that was even an issue.
With more kidneys to choose from, doctors could also more easily manage donor chains. Many people volunteer to donate a kidney to a friend or loved one in need, only to find out that they are not a compatible match. With this program, they could still donate, and the National Kidney Registry computer software would find a matching donor. One donor in the voucher program could be used to trigger a chain of transplants, creating the added benefit of freeing people from dialysis now, and their loved ones from dialysis in the future.
Potential donors often state that they are interested in donating a kidney but are hesitant because a spouse or a child could need one in the future. With the voucher program, that issue is no longer a concern.
As a transplant surgeon, I’m invigorated by the prospect of what this voucher program could mean. This could be our only realistic shot at eliminating the waiting list for kidney transplants.
Dr. Veale, a transplant surgeon at Ronald Reagan UCLA Medical Center, is director of the UCLA Kidney Transplantation Exchange Program.
Waiting
Mr Barnes’ regime is strict. The process takes him four and a half hours, it is physically demanding and it is keeping him alive.
Three years ago, Mr Barnes’ kidneys failed. He was put on an active waiting list for organ donation that would change his life.
“(Organ transplant) is something I always think about...it would certainly make a big difference in my life,” Mr Barnes said. “For me to receive a kidney, it would be from a deceased person and it is hard, but you still hope to get the call every day and it’s got to be a match.”
This year’s DonateLife Week, which started on Sunday, is themed ‘end the wait' and urges Victorians to join the Australian Organ Donor Register online.
Mr Barnes was diagnosed with polycystic kidney disease when he was 28 years old. Growing cysts would enlarge his kidney and gradually damaged the kidney tissue to the point when they failed.
Now aged 45, Mr Barnes said his life was not all doom and gloom. He maintains a healthy lifestyle and diet and has to carefully watch his fluid intake, which can often mean a fine line between dehydration and too much fluid.
As director of construction company SJ Weir, Mr Barnes works smarter by doing some paperwork on his iPad on dialysis and scheduling his dialysis in afternoons to get work done early then be fresher the next day.
Travel on short notice is tougher. Mr Barnes has to be assured he can have treatment at set times when away.
“It probably took me 12 months to get used to the way life changed with dialysis,” Mr Barnes said. “Before I was on it, I took my life for granted a bit. Dialysis really changes your life but is now part of my weekly routine.”
One third of Australians have registered their donation decision on the national donor register, despite almost 70 per cent of people indicating they would be willing to become a donor. DonateLife encourages people to talk about their decision with loved ones.
No comments:
Post a Comment